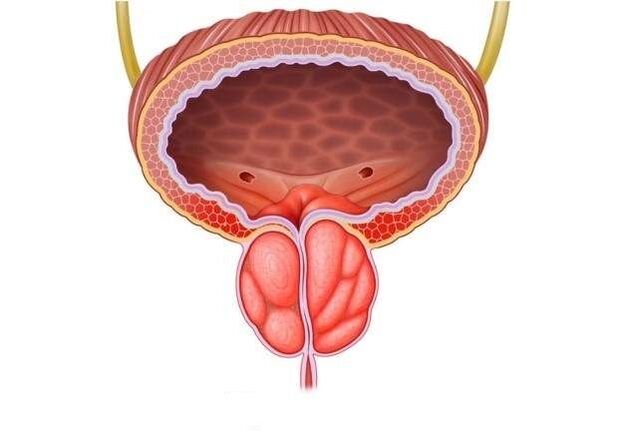
Today, inflammation of the prostate gland is the leader in the group of male diseases that are mainly sexually transmitted. Its complications threaten infertility, decreased libido and impotence.
Symptoms of prostatitis are not only pain, urinary disorders and inflammation of the spermatic cord. The most dangerous consequence of advanced inflammation can be cancerous degeneration of the prostate gland. However, the pathological process diagnosed in time is easily stopped.
Causes of inflammation
The risk of developing inflammation of the prostate increases due to various factors predisposing to the disease:
- Hypothermia associated with one-time or outdoor work.
- A sedentary lifestyle leads to disruption of the digestive system.
- Chronic somatic diseases (diabetes, hypertension).
- Focal, perifocal foci of infection (rhinitis, tonsillitis, stomatitis, gastritis).
- Persistent UGI (chlamydia, trichomoniasis, herpes virus).
- Stress, insomnia, chronic fatigue syndrome.
- Decreased immunity due to illness, surgery, emotional stress.
- Bad habits that lead to the development of intoxication: alcohol, smoking, strong coffee.
- Occupational injuries in the perineum of car drivers, athletes, workers in hazardous industries.
- Immoral sex life, interrupted sexual intercourse, loss of sensitivity with incomplete ejaculation, lack of intimacy for a long time (the lack of sperm causes stagnation in the gland).
- Venereal diseases.
Despite quite a large number of provocative points, the essence of prostatitis is the formation of stagnation in the body against the background of disruption of blood circulation and lymph flow.
Symptoms of prostatitis
Prostatitis can be suspected based on the following disorders in the work of the genitourinary system:
- discomfort while urinating, uncontrollable urination;
- impotence disorder, weak erection, decreased libido;
- difficulty urinating, a feeling of incomplete emptying of the bladder;
- pain in the perineum when sitting for a long time, for example, while driving;
- infinity.
The acute stage of the disease causes significant anxiety. This stage is accompanied by the following symptoms:
- frequent painful urge to urinate;
- delay or inability to urinate;
- throbbing pain in the perineum, transmitted to the anus and intensified during defecation. As a result, difficulty in defecation;
- general intoxication of the body, feverish condition.
The chronic form of prostatitis is accompanied by other symptoms:
- slight increase in body temperature;
- constant fatigue;
- slight pain in the perineum, burning in the urethra;
- discomfort during urination and defecation;
- weakening of sexual function and as a result psycho-emotional depression.
Classification
There is no uniform classification of the disease in modern urology. However, practicing doctors prefer this option to classify the inflammatory process in the prostate
According to the course of the disease:
- Acute prostatitis. It accounts for more than 50% of disease cases in people under the age of 30-35.
- Chronic selection. It is considered a non-age category. It does not manifest itself for a long time, the impetus for its development is a cold or infection.
For reasons that cause pathology:
- Bacterial inflammation of the prostate gland prevails in men up to 40 years of age, occurs against the background of ultrasound and does not extend beyond the limits of the organ.
- Non-bacterial pathological changes in the gland are mostly chronic.
- Viral inflammation of the prostate is characterized by an acute course that affects the entire genital region.
According to the nature of structural changes in the prostate gland:
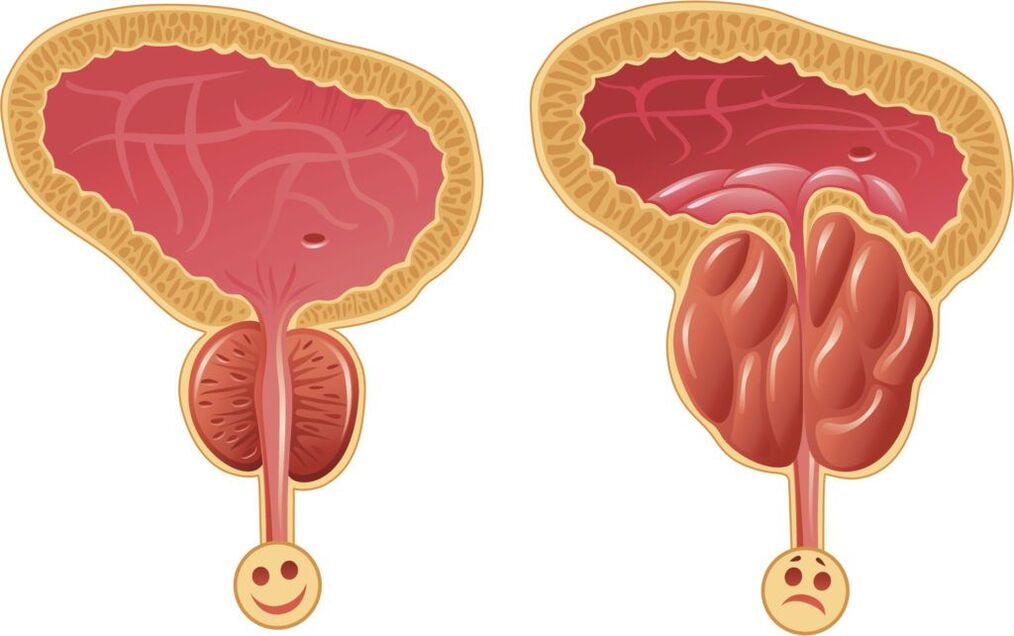
- Fibrous prostatitis is characterized by rapid irreversible growth of the gland and requires radical intervention. Clinically, it resembles prostate adenoma.
- Calcific inflammation of the prostate gland occurs due to the formation of stones inside the prostate gland. It is considered a harbinger of cancer.
- Congestive prostatitis, which is the result of a sedentary lifestyle, is diagnosed in every second patient.
Symptoms of the disease
If a man notices at least two of the following symptoms of prostatitis, he should immediately contact a qualified specialist:
- Disturbance of urination, causing an unusually short, splashing, difficulty and pain before urinating, with an intermittent, weak stream of urine. The urge to urinate frequently occurs mostly at night.
- Pain localized in the lower abdomen spreads to the scrotum, perineum and rectum.
- Sexual dysfunction.
- Problems with ejaculation, changes in sperm (consistency, quantity).
Acute prostatitis
The disease begins with a sharp increase in temperature (up to 40 degrees), painful headache, fever. Visible symptoms are accompanied by pain in the groin, perineum, back, urethral discharge, frequent urination and constant urge to urinate.
Bladder emptying occurs with delay and burning sensation. Urine itself is cloudy and may contain blood. Irritation and fatigue occur.
The result of acute prostatitis can be a complete resolution of the process (if treatment is started on time). Since changes occur in many pelvic organs, they cannot be left to chance, otherwise relevant complications will arise:
- Vesiculitis is an inflammation of the seminal vesicles, which is the cause of the formation of pus in spermatozoa, and this not only reduces the quality of ejaculation, but also leads to loss of reproductive function.
- Coliculitis - inflammatory changes in seminal tuberculosis cause the development of severe pain during sexual intercourse, cessation of orgasm and psychological impotence.
- The formation of an abscess in the body of the prostate gland, its rupture, and purulent damage to the rectum cause aggravation of symptoms, severe intoxication of the body, and even death.
- Stagnation in the tissues of the prostate causes changes in their structure, disruption of innervation, disruption of blood supply to both the gland itself and nearby organs, and disruption of its functions. Erection is insufficient for full sexual intercourse, premature ejaculation and long sexual intercourse without orgasm are observed.
- Cicatricial changes in the gland and spermatic cord lead to infertility, reduced sperm quality and sperm motility. The narrowing of the urethra prevents the normal urination process, the blockage of the bladder can cause acute urinary retention, requiring urgent surgical assistance.
Chronic prostatitis
The main feature of the disease is the uncertainty of clinical symptoms with a long, continuous course of the process. More often, the chronic form, blood stagnation in the vessels (prostatosis), occurs independently as the main pathology against the background of abacterial prostatitis.
The main symptoms of chronic prostatitis:
- temperature;
- pain occurs in the scrotum, perineum, anus, back;
- urinary disorders;
- mucous or mucopurulent discharge from the rectum, urethra, even in the absence of urine or defecation;
- erectile dysfunction, painful ejaculation, interrupted sexual intercourse, prolonged intercourse without satisfaction.
Inactivity and improper treatment of chronic prostatitis can lead to complications:
- Infertility is the result of chronic inflammation in the spermatic cord, vesicles, testicles and their appendages.
- Cystitis, pyelonephritis (other diseases of the genitourinary system) are the result of hematogenous and mechanical spread of microbes.
- Sepsis.
- Continuous decrease in immunity.
- Untreated prostatitis can lead to cancer in 35-40% of cases.
Diagnostics
The clinical picture of the disease is typical, so the diagnosis is not difficult. Medical history, examination of the patient is carried out by a urologist on the basis of the laboratory minimum using the most modern medical devices:
- Rectal examination of the gland, taking secretions for examination (culture with determination of sensitivity to antibiotics).
- UAC, UAM, bacterial culture of urine.
- Smear test for STD, UGI examination.
- Daily monitoring of the rhythm of urination, measurement of the rate of urination (uroflowmetry).
- Ultrasound or TRUS is performed for differential diagnosis.
- If it is necessary to exclude oncology, a biopsy is performed, urography is performed and PSA is determined - prostate-specific antigen.
- To diagnose infertility, a spermogram is prescribed - an analysis of ejaculation to determine a man's fertility.
Based on the results of the patient's examination, an individual scheme for the complex treatment of prostatitis is drawn up. When prescribing the drug, the form of the pathology and the presence of accompanying diseases are taken into account. The doctor decides where the treatment will be carried out (inpatient or outpatient). The course of treatment is carried out with careful laboratory monitoring of the results.

Treatment of acute prostatitis
Acute prostatitis requires bed rest, a special salt-free diet and sexual abstinence.
Course treatment methods:
- The most effective treatment of prostatitis is etiotropic therapy. If the basis of prostatitis is an infection, a course of antimicrobial agents that eliminate the manifestations of inflammation is a priority.
- Pain syndrome is eliminated with analgesics, antispasmodics, rectal suppositories, microenemas with warm solutions of painkillers. NSAIDs can be used.
- The combination of immunostimulants, immunomodulators, enzymes, vitamin complexes and trace elements has proven its effectiveness.
- Physiotherapy methods are possible only in the subacute stage of the disease. They improve microcirculation and increase immunity: UHF, microwave oven, electrophoresis, laser, magnetic therapy.
- Massage is another effective way to affect the prostate. It opens the channels, normalizes blood circulation in the scrotum and pelvis.
- Acute renal filtrate retention can be corrected by catheterization and trocar cystostomy.
- The purulent process involves surgical intervention.
- Psychologist advice.
Therapy for acute inflammation of the prostate is complex.
Effective treatment of acute prostatitis in men includes drugs from various pharmacological groups:
- Antibiotics.Drugs with a broad spectrum of activity are used, which have a bactericidal effect on most pathogens. Often, antimicrobial treatment is an etiotropic measure, because in most cases the cause of inflammation of the prostate is microbial pathogens. Antibiotics are prescribed for bacterial infection, antiviral drugs for viral infection, and anti-trichomonas drugs if protozoa are detected. The choice of antimicrobial agents is made empirically or based on the results of PCR, bacterioscopy and bacterial culture. Selection of antimicrobial agents, determination of their dose, frequency and duration of administration can only be performed by the attending physician. In addition to antibiotics, uroseptics that have a disinfecting effect on the mucous membrane of the genitourinary system can also be prescribed.
- Anti-inflammatory drugs.It allows to reduce the severity of swelling in tissues and the intensity of pain. As a rule, non-steroidal anti-inflammatory drugs (NSAIDs) are used for this.
- Intravenous drugs- reduces tissue swelling, removes congestion in the prostate, thereby helping to reduce pain, improve blood circulation in tissues and local metabolic processes.
- Enzymes- thins the prostate secretion and promotes the flow of pus. In addition, enzymatic preparations increase the effectiveness of antimicrobial treatment by improving the absorption of their active substances by the affected tissues.
- Diuretics (diuretics).They increase urination, which helps to mechanically "wash" the infection.
- When taking antibiotics, patients are prescribed hepatoprotectors that protect the liver parenchyma from toxic damage and improve its functional state.
- Patients are prescribed probiotics to prevent and prevent the development of intestinal dysbiosis during antibiotic therapy.
- After the reduction of acute inflammatory phenomena in the prostate gland, patients are prescribed a course of physiotherapeutic treatment - drug electrophoresis, galvanization, magnet, laser, mud therapy, etc. Such procedures improve local microcirculation and lymphatic drainage, metabolic processes and tissue nutrition, stimulate tissue repair, accelerate the final resolution of the inflammatory process, help restore tissues and normalize the functional state of the prostate.
General activities should be carried out.
For acute prostatitis in men, a diet, including a sufficient supply of easily digestible proteins and vitamins, is indicated.
During the exacerbation of inflammation, spicy, fried, fatty, salty foods and marinades are excluded from the diet.
Alcohol consumption is excluded, abstinence from smoking, abstinence from sexual intercourse and intensive physical activity, including sports, are recommended.
It is necessary to normalize sleep, work and rest, balance the emotional background.
During illness, a person needs functional rest.
With timely, correct diagnosis and treatment of acute prostatitis in a medical institution, the prognosis is favorable - full recovery occurs.
If acute prostatitis develops, consult a doctor immediately and do not self-medicate!
Treatment of chronic prostatitis
There is no 100% guarantee of treatment with a long-term, course (at least one month) effect on the prostate gland. Priority is given to herbal medicines, immunocorrection, changing household habits:
- Herbal preparations are widely used in urological practice. They can accumulate at the site of the most active pathological process, protect cells from oxidation, remove free radicals and prevent the proliferation of glandular tissue.
- Antibacterial therapy is selected individually based on the sensitivity of microbes to drugs.
- Medicines that strengthen immunity not only help to cope with prostatitis, but also correct the negative effects of antibiotics that disrupt the function of the immune system.
- The pain syndrome is relieved by taking alpha-blockers and muscle relaxants.
- Prostate massage allows you to mechanically remove the "extra" secretion of the gland through the urethra, improve blood circulation and minimize blockage.
- Physiotherapy: laser, magnet, ultrasound, iontophoresis, hot sitz baths or microenemas with herbs.
- In severe cases, intravenous fluids with diuretics are indicated. It stimulates the production of abundant urine, prevents the symptoms of intoxication, the development of ascending cystitis and pyelonephritis.
- Herbal laxatives are used for constipation.
- Together with the patient, the urologist and psychologist develop an individual long-term program of daily routine, necessary rest, diet, dosed physical activity and sexual activity.
- If the chronic process is resistant to therapy and the flow of urine is blocked, surgical intervention is prescribed: removal of all affected tissues (transurethral resection of the prostate) or complete removal of the gland with surrounding tissues (prostatectomy). It is applied in exceptional cases, it is fraught with impotence and urinary incontinence. Young people are not operated on because it can cause infertility.
Treatment with drugs
The treatment of prostatitis with antibacterial therapy should start with a bacterial culture, the purpose of which is to assess the sensitivity of the body to this type of antibiotic. If urination is disturbed, the use of anti-inflammatory drugs gives good results.
Medicines are taken in tablets, in acute cases - by drops or intramuscularly. Rectal suppositories are effective for the treatment of chronic forms of prostatitis: with their help, drugs reach their goals faster and have a minimal effect on other organs.
Blood thinners and anti-inflammatory drugs have also proven to be effective.
Antibacterial therapy
Antibiotics are an effective tool in the fight against bacterial prostatitis. In order to achieve the desired effect and not harm the body, the choice of medicine, dosage and treatment regimen should be carried out by a doctor. In order to correctly choose the most effective drugs, he must find out what kind of pathogen causes prostatitis, and also test the patient for tolerance to antibiotics of a certain group.
Antibiotics from the fluoroquinolone group have proven themselves in the treatment of chronic prostatitis. Their action is aimed at preventing bacterial infection and strengthening the body's own immunity. In addition, the bacteriostatic antibiotic trimethoprim is recommended for the prevention and treatment of accompanying diseases of the genitourinary system.
Prostatitis caused by mycoplasma and chlamydia can be additionally treated with drugs from the group of macrolides and tetracyclines, which slow the spread of infection.
The duration of taking antibacterial drugs is from 2 to 4 weeks. In case of positive dynamics, the course can be extended.
Physiotherapy
Physiotherapy methods in the treatment of prostatitis are aimed at activating blood circulation in the pelvis, improving metabolic processes in the prostate gland, and cleaning the channels. If physiotherapy is combined with taking antibiotics, the effect of the latter is strengthened.
The main methods include:
- magnetic therapy;
- laser therapy;
- electrophoresis;
- warming up;
- ultrasound;
- mud treatment;
- high frequency radiation;
- physiotherapy.
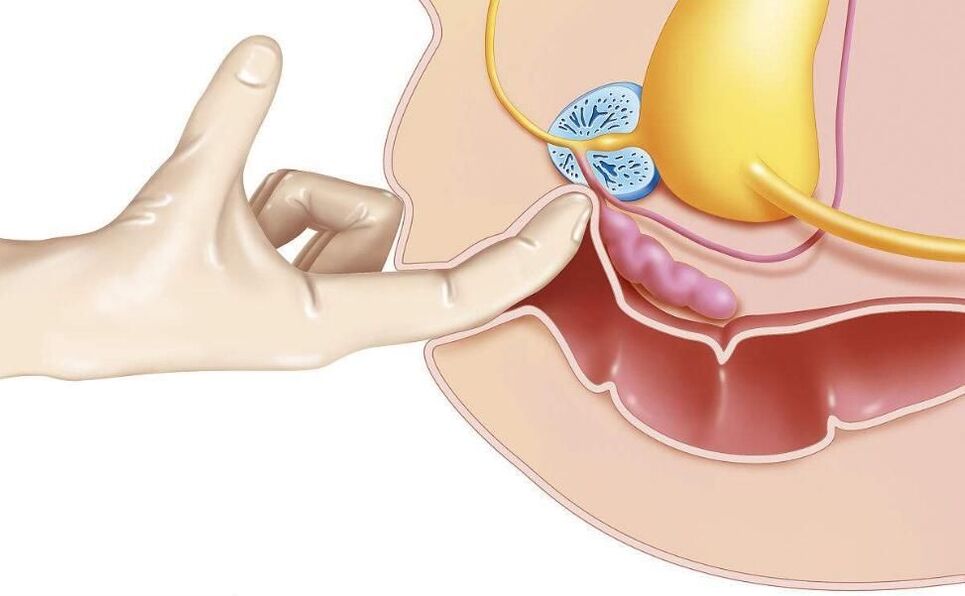
One of the oldest methods, transrectal massage of the prostate gland, according to modern research, has no proven effectiveness.
Non-specific treatments
Non-specific treatments for prostatitis include:
- hirudotherapy;
- therapeutic fasting;
- acupuncture;
- Diet according to the Ostrovsky method;
- Alkalization of the body using the Neumyvakin method.
We strongly recommend that you discuss all non-traditional methods of prostatitis treatment with your doctor.
Surgery
Surgical methods are used in complicated and urgent cases:
- for drainage of purulent abscesses removed by laparoscopic methods through puncture;
- when it is difficult to urinate due to damage to the urinary tract;
- with a large volume of the affected area;
- with a significant number of stones in the body of the gland.
Stones and sclerotic tissues are removed endoscopically. If the affected area is large or there are many stones, resection of the prostate gland is used.
Transurethral resection is also effective in bacterial prostatitis. In this way, the risk of relapse can be reduced.
Folk treatment

Treatment of prostatitis with folk remedies is unlikely to be effective on its own, but it can be used in combination with drugs and physiotherapeutic methods. These include: beekeeping products, decoctions of herbs and seeds, garlic, ginger, beaver flow, fresh vegetables, pumpkin seeds.
In acute cases of the disease, you must consult a doctor and do not self-medicate under any circumstances! If the purulent abscess ruptures, death is possible.
Candles for prostatitis
Treatment of prostatitis with rectal suppositories is more effective than tablets, if the rectum is closer to the prostate, this means that the medicine will act faster.
The composition of drugs for the treatment of prostatitis can be completely different, they are prescribed to solve a specific problem.
- Antibacterial agents are particularly effective for prostatitis caused by chlamydia.
- Painkillers are used for symptomatic treatment, they relieve pain well.
- Immunostimulants help improve blood circulation, remove swelling and are used in complex therapy.
- Herbal medicines have a mild effect. They are used in addition to the main treatment, like candles on bee products.
- Ichthyol-based compositions promote blood flow in the region of the intestinal mucosa, which accelerates the weakening of inflammatory processes and slightly improves immunity.
- Products based on special enzymes prevent the formation of scar tissue. It is recommended to take it as part of complex therapy with antibiotics, anti-inflammatory and pain relievers.
Auxiliary drugs
For the symptomatic treatment of prostatitis in men, for example, to relieve pain when urinating, in addition, you can take antispasmodics that relax smooth muscles and thereby quickly relieve pain.
Overall health is enhanced with blood thinning and anti-inflammatory dietary supplements based on bee products, pumpkin seed oil and palm fruit extracts.
Diet and lifestyle
A proper, balanced diet and a healthy lifestyle are very important for the treatment of prostatitis. Food should not contain spicy, fried, salty or acidic foods. In severe cases, alcohol is strictly prohibited.
Food should contain enough fiber to prevent constipation. The amount of protein should be reduced. It is recommended to add herbs, ginger and pumpkin seeds to the diet.
Consequences of untreated prostatitis
Even if the symptoms of prostatitis do not appear for a long time, it is necessary to undergo regular examination by a urologist. Completely untreated prostatitis can be accompanied by the formation of calcifications, which will then have to be removed together with the gland. Experts are sure that there are no other methods to remove or dissolve stones.
In addition, pathogenic microorganisms can migrate to neighboring organs, causing inflammation. Advanced prostatitis can lead to the development of adenoma and prostate cancer.
Prevention
To prevent the occurrence of an unpleasant disease for men, it is necessary to eliminate provoking factors and follow simple rules:
- Lead a healthy lifestyle, give up bad habits.
- Do not get too cold.
- Drink at least 1. 5-2 liters of water per day.
- Strengthen your immune system, walk a lot, get tough.
- Do physical education and sports, visit fitness clubs.
- Avoid stressful situations.
- Have regular sex with a regular partner.























